Patient Journal of Nursing

The Impact Of Implementing A Patient-Centered Medical Home Model In The Primary Care Setting
Tags: care health patient Primary Care
Literature demonstrates a trend of shared decision-making models that are centered around the patient. By implementing the Patient Centered Medical Home (PCMH) model, patient encounters will encompass a patient-centered decision-making approach regardless of the reason for the visit. This model incorporates ongoing preventative screenings into routine visits to create a continuum of meeting wellness initiatives without relying on a routine wellness visit yearly. To implement this model, the clinician will thoroughly review the patient’s chart prior to the office visit. If any preventive screening is identified, then the primary care provider addresses the initiatives during the encounter. Post-implementation data showed a marked increase in ordered preventive screenings, wellness exams, and revenue to the clinic. There was also an increase in patient satisfaction perception among participating providers. The PCMH model allows the clinician avenues to address, create dialogue, and implement shared decision-making to incorporate preventative screenings and keep preventive care moving forward.
Read More →
Crohn’s Disease
Tags: Chron's disease patient symptoms treatment
The paper includes the identification, etiology, diagnosis, and treatment of Crohn's disease. The paper also addresses nutrition, diet, and nursing interventions and education to help manage the disease.
Read More →
Rapid Response Team to the Rescue
Tags: Ambulance cardiac Doctors EMS Follow-Ups patient patient safety Rapid Response rapid response team rapid response team benefits Rescue Rescue Team RRT RRT Nurse RRT Nursing Team treatment working together
Rapid response team (RRT) purpose is to initiate immediate measures before patient deteriorates further and to educate the staff on activating the staff the Rapid response team.
Read More →
Nurse/Patient Communication Twenty Suggestions for Improvement
Tags: communication improvements nurse patient twenty
From time to time, physicians are taken to task by fellow physicians and many others for a variety of shortcomings in the practice of their profession. Common among the listed faults is a lack of effective communication with their patients.
Read More →
The Importance of Communication and Education toward Patient Literacy: The Relationship of Functional Health and Patient’s Knowledge of Their Chronic Disease and Metabolic Disorder
Tags: aging assessment skills clear with simplified language communication communicator diabetes direct involvement disease educator efficiency of care health health literacy knowledge patient patient education
The aging populations in the U.S. with ‘Essential’ Hypertension are showing inadequate health literacy, plus its impact on patients with idiopathic chronic diseases such as type II, adult onset Diabetes Mellitus are makeable. To identify among patients with hypertension and/or with diabetes the relationship between their functional health literacy levels, and the role of the registered nurse as communicator and educator.
Read More →Get Published for Free
Browse by Tag
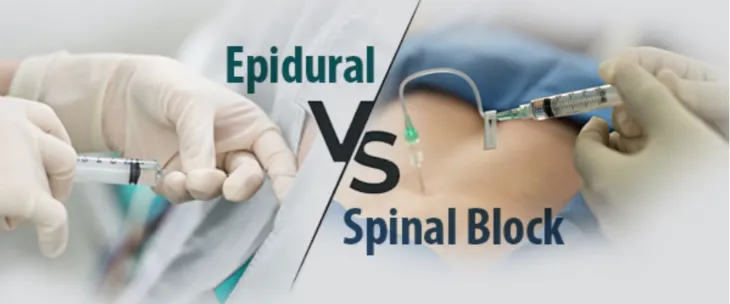
advocate aging anesthesia behavior cancer cardiac care Case Study child children clinical COVID-19 critical care death diabetes disease education emergency department end of life ethical principles ethical values ethics graduates health health care ICU medication mental health nurse Nurse Education nursing nursing ethics nursing faculty nursing school nursing students PACU patient care patient outcomes patient safety pediatric pediatrics poem risk factors stress student nurse students teaching therapy treatment violence
Most Popular Last Month
More from RN Journal
Maladaptive Strategies and Self-Harming
Conflict Resolution
Going Against the Norm: Treating Cancer as a Metabolic Disease
First Day of Kindergarten
Love hate relationship in nursing
A Study To Exploring Nursing Students’ Lived Experiences In Pediatric Clinical Practice In A Selected College, Chennai
Detour Off The Sepsis Road: Early Recognition is Key
The Cardiac Diagnostic Interventional Symposium (CDIS)
A nursing-driven approach towards reducing hypertension: a focus on evening dosing and circadian rhythm