Why Skin Tears Are a Big Deal
Submitted by Donna Boyer, RN, WCC
Tags: cellulitis dermatitis pressure ulcers reduced wound healing skin skin infections skin tears

I overheard a conversation between a nurse and a provider who commented, “It’s not a big deal, it’s just a skin tear”. Having recently been introduced to the International Skin Tear Advisory Panel’s (ISTAP) resources, I felt compelled to explain exactly why skin tear development is, indeed, a very big deal.
The first thing that came to my mind was the impact that this injury may have on the patient’s overall comfort and well being. This type of traumatic injury may cause physical pain as well as having the potential to inflict psycho-social harm. Could this physical discomfort cause her to withdraw from activities she usually enjoys participating in? Would she be self conscious about the bandage on her arm or the discoloration of her skin that was caused by the trauma? It made me wonder, ‘How would I cope with this type of injury’?
Skin tears can occur on any part of the body, but are most often found on the extremities, such as upper or lower limbs or the dorsal aspect of the hands. Skin tears are acute traumatic wounds that are caused by mechanical forces. Those mechanical forces may include the removal of adhesives (Medical Adhesive Related Skin Injury - MARSI). Skin tears are the most common wound type in the elderly population, although skin tears can be seen in individuals of all ages. Therefore it’s important for clinicians, in all care settings, to be aware of risk factors, interventions to mitigate those risks and appropriate treatments. These types of injuries have a high risk of becoming complex wounds, and, of course, anytime there is a break in the skin’s integrity, there is an increased risk of infection.
A comprehensive skin assessment should be conducted on admission with ongoing, daily inspection of the skin to identify changes in condition as soon as possible. Remember that very often a skin injury is an outward sign of an internal issue. The International Skin Tear Advisory Panel’s (ISTAP) 2020 Best Practice Recommendations for Holistic Strategies to Promote and Maintain Skin Integrity document contains a very helpful guide on recognizing potential skin problems based on the patient’s overall frailty. I personally found this tool very helpful in reminding me to take a holistic approach when identifying risk factors for skin injury, looking at both extrinsic and intrinsic factors.
Patient groups at risk for skin frailty (adapted from Wounds UK, 2018)
| Patient Group | Skin Changes | Potential Problems |
| Older adults | Becomes thinner, loses elasticity, reduced blood supply, subcutaneous fat decreases, skin hydration decreases, reduction of the dermal-epidermal layer (diminishing adherence of epidermis on dermis; Moncrieff et al, 2015; Levine, 2020) |
Skin tears, pressure ulcers, infection, inflammation, dryness/flaking, itching, cellulitis, diabetic ulcers, possible nutrition issues; possible issues relating to dementia |
| Individuals with mobility issues/paralysis | Alterations to vascular supply, temperature control, maceration/moisture, loss of collagen, lack of muscle/atrophy, impaired sensation due to damaged nerves in the skin (Rappl, 2008) | Skin tears, pressure ulcers, infection, inflammation |
| Children/neonates | Immature skin; intrinsic changes due to pressure duration, shear and friction, poor perfusion and maceration (Inamadar & Palit, 2013) |
Nappy/diaper dermatitis, skin tears, pressure ulcers |
| Individuals with spina bifida and cerebral palsy | Decreased skin perfusion, cutaneous reaction to drugs, perineal dermatitis and inflammation due to incontinence (Inamadar & Palit, 2013) | Pressure ulcers; possible incontinence-associated dermatitis |
| Bariatric patients | Altered epidermal cells, increased water loss, dry skin, maceration, increased skin temperature, and reduced lymphatic flow and perfusion (Shipman & Millington, 2011) | Pressure ulcers, skin tears, diabetic ulcers, psoriasis, moisture lesions, intertrigo |
| Oncology patients | Radiation leads to inflammation, epidermis damage, decreased perfusion (NHS, 2010) | Pressure ulcers, reduced wound healing, skin infections, cellulitis, radiodermatitis |
| Chronic illness and other issues | Skin changes due to chronic illnesses - e.g. >renal, liver, cardiovascular; medications; malnutrition; stomas and devices; psychosocial issues (Wounds UK, 2018) |
Skin tears, pressure ulcers, infection, inflammation, moisture lesions; other related issues |
For those risks that can be mitigated, implement patient-specific interventions. As with all interventions, it’s imperative to include your patient in the decision making process to help ensure compliance.
One of the most effective prevention strategies is to maintain overall health. Encouraging hydration, nutrition, mobility and mental health are key factors to keeping skin healthy and intact. Another strategy that may seem simple, but is very effective, is applying moisturizer twice a day. A randomized controlled trial evaluated the effectiveness of a twice-daily moisturizing regimen as compared to 'usual' skin care for reducing skin tear incidence in a long term care facility. This study found that application of a commercially available, standardized pH neutral, perfume free moisturizer on the extremities, applied twice daily, reduced incidence of skin tears by almost 50%. If twice daily moisturizing is not currently in your at-risk-patients’ care regimen, please consider implementing it right away. The potential to reduce almost half of all skin tears may be possible. Think about the positive impact this may have on your patients!
A type of skin injury that I have recently become more aware of is Medical Adhesive-Related Skin Injuries (MARSI). MARSI can often be prevented by consistently incorporating these strategies into your routine wound care practice. You need to consider not just the removal of the dressing but also the application. Here are some practical suggestions:
- Consider using an atraumatic dressing, such as silicone
- Remove all dressings slowly, not pulling up and away but peeling the dressing away keeping it low, next to the body
- I don’t see this next suggestion used very often, but I think it has the opportunity to make a significant difference. Mark the dressing with an arrow to indicate the correct direction of removal. This could possibly preserve a skin flap or prevent further injury to already damaged skin
- Prior to dressing application use a skin barrier to reduce trauma when the dressing is removed
- Use adhesive removers to loosen the bond between the dressing and the skin
- Use the appropriate size adhesive dressing to decrease the amount of peri-wound skin coming into contact with the adhesive dressing
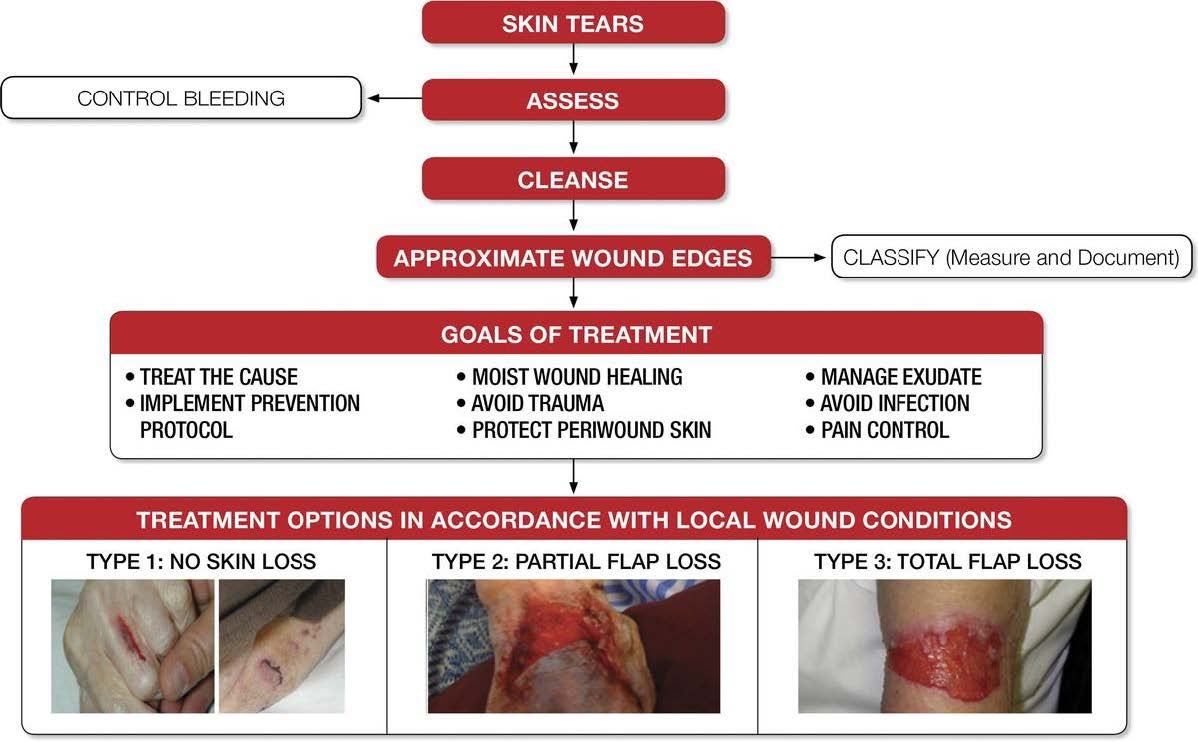
If, unfortunately, a skin tear occurs, there are three commonly utilized skin tear classification systems. The Payne Martin Scale, ISTAP (International Skin Tear Advisory Panel) and STAR (Skin Tear Audit Research). Determining which system is used in your organization is essential to ensure consistent understanding of the extent of the injury. You can find detailed information regarding these classification systems on the ISTAP web site at www.skintears.org.
Appropriate treatment for skin tears, like any wound type, is essential in promoting wound healing. By utilizing ISTAP’s Tool Kit (www.skintears.org) you can ensure you are following current standards of practice for treating these injuries.
I encourage every clinician to check out the many valuable resources, including education presented by international content experts, that are available on the ISTAP website. Membership is complimentary. www.skintears.org
By increasing our awareness of the vital importance of skin, and looking at our patient’s risk factors holistically, we have a huge opportunity to not only improve outcomes but, most importantly, improve our patients’ quality of life.
References:
- ISTAP 2020 Best Practice Document: “Holistic strategies to promote and maintain skin integrity”
- ISTAP: Evidence Based Prediction, Prevention, Assessment, and Management of Skin Tears Poster