Using Virtual Reality Simulation as a Tool to Improve Clinical Competencies
Submitted by Lynette DeBellis, EdD, RN, CNE and Stacia Donaldson, MBA, RN, CHSE, CHSOS
Tags: Nurse Education virtual learning virtual professor

ABSTRACT
Simulation has long been recognized as an effective instructional method in nursing education. The use of virtual reality simulation as compared with traditional simulation, adds a new dimension to the complexity of simulated patient care. In this study, students’ perceptions of improved clinical competencies such as confidence, priority setting, delegation, time management, and communication were evaluated using a post simulation survey and reflective journaling. Results demonstrated an improvement in clinical competencies.
Keywords:
nursing education, simulation-based learning, virtual reality (VR) simulation, clinical confidence, priority setting, clinical decision-making.
BACKGROUND
The use of simulation in nursing education as a pedagogical method to provide a real-life experience in a safe, controlled environment has been available for decades (Bradley et al., 2025) in nursing and healthcare education. Various types of simulations have emerged over time. These variations include high-fidelity simulation, human patient simulation, virtual simulation and virtual reality. Hands-on simulation provides the student with an opportunity to make clinical judgments and review their actions during debriefing sessions. The use of virtual reality, with accompanying tools, may provide the student with an experience that more closely mimics the real-life clinical experience. (Bradley et al., 2025).
However, there remains a gap in evidence regarding its impact on clinical decision making and outcomes.
Simulation provides nursing students with an opportunity to learn clinical skills, make clinical decisions, and collaborate with the interdisciplinary team in a secure and structured environment (Koukourikos et al., 2021) The authors suggest that simulation significantly helps nursing students assimilate into the role of successful health care professionals.
In a study conducted by Li et al. (2022), the authors concluded that high-fidelity simulation can successfully promote knowledge, collaboration, caring, and interest in learning in undergraduate nursing students. Furthermore, high-fidelity simulation was equal to other teaching methods to promote critical thinking and self-confidence.
In their review of the literature and subsequent meta-analysis of over three hundred students, Hemlata, & Trivedi (2023) reported that simulation enhanced nursing students’ cognitive, affective and psychomotor skills. They suggest that simulation must be part of every nursing curriculum to produce efficient clinical nurses.
Saab et al. (2021) report that students felt virtual reality simulation was ‘captivating’ ‘engaging’ and enhanced confidence. Foronda et al. (2024) report that both traditional and virtual reality simulation provide effective methods for learning experience in healthcare professions students.
Research conducted by Kiegaldie & Shaw (2023) demonstrated that students perceived virtual reality to be realistic and less intimidating than typical simulation. Additionally, students reported that critical thinking skills were developed as a result of participating in the virtual reality simulations. Similar to findings of Choi et al. (2022), students reported that technical issues such as wearing the headset or VR glasses and simulation sickness were restricting factors.
METHODS:
As part of the curriculum plan, senior nursing students at a small, private liberal arts college, take an advanced Medical-Surgical/critical care course focused on complex health problems, as their last clinical course before graduation. This course is 6-credits, providing three hours of lecture per week, and 10 hours of clinical per week. Due to anticipated lack of clinical placements and clinical faculty, the simulation manager and the Chair of the School of Nursing developed a proposal to increase the number of simulation hours/percentage from 10% to 30%. Although this percentage was within the acceptable range, approval was required by the State Department of Education-Office of the Professions since is constituted a change from our original plan of study. Once approval was secured, the proposal was implemented for 105 senior nursing students.
Our study sought to determine if senior level nursing students who participated in virtual reality simulation would report an increase in confidence in clinical competencies in areas such as clinical judgment, priority setting, and delegation after three sessions.
All students were required to view the VR clinical tutorial prior to the first assignment. Each student received training with the VR headsets. Three students were unable to continue with the headsets and were given the opportunity to complete the assignments on a laptop.
Students participated in one traditional simulation with a rapid response patient as well as three virtual reality experiences. Learning objectives were developed for each assignment. Each VR experience increased in the number of patients cared for by the student as well as the acuity of patients. The scenarios represented a typical day in a virtual emergency room. The entire experience for each VR assignment spanned approximately three-hours in length and included pre-briefing and debriefing with the simulation manager/nurse educator. Students were encouraged to journal their experiences as they progressed through the assignments.
Results
One hundred five students were given the opportunity to participate in a post-experience survey to
evaluate the virtual reality simulation clinical experience. The survey was approved by the College’s IRB, and participation was voluntary. Overall, students reported a positive experience with VR simulation clinical. Students experienced an increase in confidence, ability to prioritize care, and they were able to delegate more effectively by Assignment #3. (Figure #1, Figure #2). Sixty percent of the students reported that Assignment #3 helped them achieve an overall better outcome. Sixty percent reported that Assignment #3 improved their ability to prioritize. Interestingly, students reported both Assignments #2 and #3 improved their ability to delegate equally. Sixty percent of the students reported that Assignment #3 improved their time management skills. Seventy percent of the students reported that Assignment #3 improved communication skills. One hundred percent of the students reported that the most helpful part of the experience was caring for multiple patients. Ninety percent of students rated as ‘second most helpful’ receiving ‘real-time’ interruptions and providers’ calls while caring for patients. Students felt this represented an accurate clinical experience.
In regards to technology, ninety percent of the students reported that the VR controls were the most challenging to deal with.
Figure #1
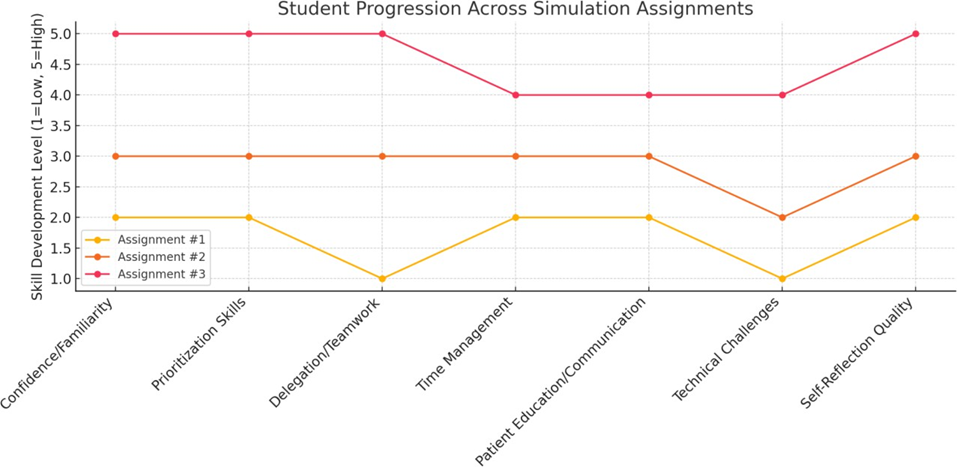
Figure #2
|
Category |
Assignment #1 |
Assignment #2 |
Assignment #3 |
|
Confidence and Familiarity |
Low to Moderate. Students adjusting to VR technology, many technical frustrations. |
Moderate. Most students reported better navigation and confidence with VR |
High. Students were much more comfortable and focused on clinical skills, not technology. |
|
Prioritization Skills |
Emerging. Students mostly recognized correct patient priority but sometimes hesitated or second-guessed. |
Improved. Students applied prioritization frameworks and began anticipating next steps. |
Strong. Students showed confident prioritization even when handling simultaneous emergencies. |
|
Delegation and Teamwork |
Minimal. Some students delegated, but many forgot or were unsure. |
Increasing. More students used UAPs/RNs appropriately but occasionally forgot to verify completion. |
Well-Developed. Delegation was integrated into workflows, helping students handle complex cases. |
|
Time Management |
Challenging. Poor pacing and frequent feelings of being overwhelmed. |
Improving. Students developed task lists and organized care better, though some still struggled. |
Considerably improved. Students handled time pressures better, even during high-acuity events. |
|
Patient Education and Communication |
Often missed. Focus was task completion, not holistic patient care. |
Growing awareness. Students began recognizing need for better patient teaching. |
Stronger emphasis. Students consciously incorporated patient education and communication. |
|
Technical Challenges |
High. VR headset discomfort, controls confusion, simulation glitches. |
Moderate. Still some technical barriers, but fewer interruptions to clinical performance. |
Low. Only minor issues reported, mostly technical "quirks," not barriers. |
|
Self-Reflection Quality |
Fundamental. Students noted broad areas for improvement (navigation, organization). |
Deeper. Reflections became more detailed (e.g., specific missed assessments, task prioritization). |
Insightful. Students identified subtle clinical judgment growth and areas for continued improvement. |
Interpretation
The VR simulation clinicals were implemented as a teaching method when it became evident that there was a shortage in the number of critical care clinical sites available for senior nursing student placement. The faculty was concerned about replacing clinical hours with simulation hours. However, as noted in Figure #1 and Figure#2, senior nursing students reported an increase in confidence from low-moderate to high from assignments one to three, respectively using this planned alternative learning method. In addition, students reported prioritization skills improving from “emerging” to “strong” by the end of assignment three. Delegation, team work, and time management skills also improved with each assignment. Interestingly, students reported improved communication skills including those required for patient education with the VR simulation clinicals.
Technical challenges improved but remained throughout the experience. The VR controls, headsets, and navigation of the program were mentioned in the survey as specific challenges.
The students’ self-reflection through journaling became deeper and more insightful by the end of assignment three. Students were able to compare and contrast the three experiences and note both personal and professional growth.
Limitations
Limitations of this study were the sample size. One hundred five students were in the study. Additionally, only senior level nursing students used VR. Technical “glitches” were problematic and will be reviewed and addressed if the same product is used in the future
Conclusion
Virtual reality simulation should be implemented and evaluated as an integrated methodology across the curriculum. From sophomore to senior level students, comparison of ability to set priorities, achieve confidence, and improve communication will be the most important areas to evaluate.
REFERENCES
Bradley, C. S., Loomis, A., DiClemente, L., Flaten, C., Rahman, S., Muehlbauer, M. K., Johnson, K., Mathiason, M., & Aebersold, M. (2025). Enhancing nursing competence and knowledge: Evaluating the impact of immersive virtual reality in nursing education. Journal of Nursing Regulation, 16(1), 2–9. https://doi.org/10.1016/j.jnr.2025.04.003
Brown, K. M., Swoboda, S. M., Gilbert, G. E., Horvath, C., & Sullivan, N. (2022). Integrating virtual simulation into nursing education: A roadmap. Clinical Simulation in Nursing, 72, 21–29. https://doi.org/10.1016/j.ecns.2021.08.002
Chen, F.-Q., Leng, Y.-F., Ge, J.-F., Wang, D.-W., Li, C., Chen, B., & Sun, Z.-L. (2020). Effectiveness of virtual reality in nursing education: Meta-analysis. Journal of Medical Internet Research, 22(9). https://doi.org/10.2196/18290
Choi, Jeeyae PhD, RN; Thompson, C Elise PhD, RN; Choi, Jeungok PhD, MPH, RN; Waddill, Colette
B. DNP, MSN, RN; Choi, Soyoung PhD, RN. Effectiveness of Immersive Virtual Reality in Nursing Education: Systematic Review. Nurse Educator 47(3): p E57-E61, May/June 2022. | DOI: 10.1097/NNE.0000000000001117
Foronda, C. L., Gonzalez, L., Meese, M. M., Slamon, N., Baluyot, M., Lee, J., & Aebersold, M. (2023). A comparison of virtual reality to traditional simulation in Health Professions Education. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 19(1S). https://doi.org/10.1097/sih.0000000000000745
Havola, S., Haavisto, E., Mäkinen, H., Engblom, J., & Koivisto, J.-M. (2021). The effects of computer- based simulation game and virtual reality simulation in nursing students’ self-evaluated clinical reasoning skills. CIN: Computers, Informatics, Nursing, 39(11), 725–735. https://doi.org/10.1097/cin.0000000000000748
Kiegaldie, D., Shaw, L. Virtual reality simulation for nursing education: effectiveness and feasibility. BMC Nurs 22, 488 (2023). https://doi.org/10.1186/s12912-023-01639-5
Koukourikos, K., Tsaloglidou, A., Kourkouta, L., Papathanasiou, I., Iliadis, C., Fratzana, A., & Panagiotou, A. (2021). Simulation in clinical nursing education. Acta Informatica Medica, 29(1),15. https://doi.org/10.5455/aim.2021.29.15-20
Li, Y. Y., Au, M. L., Tong, L. K., Ng, W. I., & Wang, S. C. (2022). High-fidelity simulation in undergraduate nursing education: A meta-analysis. Nurse education today, 111, 105291. https://doi.org/10.1016/j.nedt.2022.105291
Liu, K., Zhang, W., Li, W. et al. Effectiveness of virtual reality in nursing education: a systematic review and meta-analysis. BMC Med Educ 23, 710 (2023). https://doi.org/10.1186/s12909-023-04662-x
Mishra, R., Hemlata, & Trivedi, D. (2023). Simulation-based learning in nursing curriculum- time to prepare quality nurses: A systematic review and meta-analysis. Heliyon, 9(5), e16014. https://doi.org/10.1016/j.heliyon.2023.e16014
Mohamad M. Saab, Josephine Hegarty, David Murphy, Margaret Landers, Incorporating virtual reality in nurse education: A qualitative study of nursing students' perspectives, Nurse Education Today, Volume 105,2021, 105045, ISSN 0260-6917, https://doi.org/10.1016/j.nedt.2021.105045.