Family Journal of Nursing

The Career Path of a Family Nurse Practitioner: A Journey of Care and Compassion
Tags: care career compassion family family nurse practitioner profession
The role of a Family Nurse Practitioner (FNP) is both dynamic and rewarding, offering a unique blend of expertise and care. As healthcare continues to evolve, FNPs play a crucial role in providing comprehensive primary care to individuals and families across the lifespan. This article explores the career path of a Family Nurse Practitioner, outlining the educational requirements, job responsibilities, and potential career opportunities.
Read More →
A Husband's Difficult Decision
Tags: bedside reporting end of life family Family Presence PACU sepsis
A husband's difficult decision regarding his critically ill wife and DNR status
Read More →
When "Old Dogs" go Back to School
Tags: Bachelor's degree education family nursing leadership PACU stress
I went back to college at the age of 62. Being an "old dog", I was not computer savvy, so taking classes mostly on-line was quite challenging. I believe that my trials and triumphs evidenced in this article, will encourage nurses, especially older nurses, to go back to school for their BSN.
Read More →
The Other Side of Healing
Tags: cancer death end of life family oncology patient experience
A glance back at how I came to appreciate the special role a nurse plays in helping patients experience a peaceful death and assisting family members through the experience.
Read More →
My Pet Rock and Other Fictions
Tags: brain damage Disabilities family
Mother of son with severe disabilities explaining to her daughter why parents never divorced as they & the family experienced the tragedy of a brain damaged son.
Read More →
Advocacy for Those without a Voice: Helping Parents with Smoking Cessation
Tags: cessation child children family pediatric pediatrics second-hand smoke smoking smoking cessation
The purpose of this manuscript is to summarize current research in the area of second-hand smoke exposure in children and smoking cessation interventions for their parents.
Read More →
The Blessing: A Nurse's Story
Tags: blessing compassion family nursing stroke
It was nine o’clock pm and I was walking briskly out of Recovery Room, knowing I had to be back the next day at six am. Though in a hurry, I purveyed the family waiting room to see if there were any visitors who needed help after the patient representative had gone home. I immediately noticed a lone woman with an anxious look on her face. As it turned out, her daughter-in-law had just been transferred to Intensive Care. Instead of waiting for one of our transporters, I decided to take her up myself. As we headed down the hall, she stated: “I bet you’re trying to leave, aren’t you?” I affirmed her observation. I added that, it was quite all right. We arrived at the particular ICU where her daughter-in-law was transferred, and upon talking with the patient’s RN, I was able to let her in right away. She turned to me and said: “Thank you; you will be blessed.”
Read More →
Family Presence During CPR in the Emergency Department
Tags: Bedside Manner cpr critical care emergency emergency department Emergency nurse family Family Presence nurse
A descriptive survey conducted in 2000 (Myers, et al 2000) investigated attitudes and beliefs of patients’ families and ER staff members about FWR. The survey reported that 98% of patients’ families indicated that they had a right to be present and would do it and would participate in FWR again; 100% of family members said that FWR was helpful to them, and 95% said it was helpful for the patient. It also showed that 70% of professionals surveyed after their participation in FWR actually produced a higher level of “professional” behavior along with a more “professional” bedside dialog amongst the health care team. The survey also indicated that having the family in the resuscitation room prompted the staff to take the patient’s dignity, privacy, and need for pain management into greater consideration when compared to an un-witnessed resuscitation effort. (Myers, et al 2000)
Read More →
My Father the Medicine Man
Tags: eastern medicine family health western medicine
My father continues to avoid western medicine as much as he can and there is no convincing him any different. I only hope that the next key given to me will open a door where Eastern and Western medicine will compliment each other. Health care would have the best of both worlds if this would happen.
Read More →Get Published for Free
Browse by Tag
advocate aging anesthesia behavior cardiac care Case Study child children clinical compassion COVID-19 critical care death diabetes disease education emergency department end of life ethical principles ethical values ethics future of nursing health health care ICU medication mental health nurse Nurse Education nursing nursing education nursing ethics nursing faculty nursing school nursing students PACU patient care patient outcomes patient safety pediatric poem profession risk factors stress student nurse students teaching therapy treatment
Most Popular Last Month
More from RN Journal
Sleep Deprivation of Nurses: Poor Health Care Practice
"What is it with you?"
Clinical Nurse Leadership and Performance Improvement on Surgical Unit
Use Critical Thinking: It takes Only a Second for an Error to Occur
Do Nurses Need Biology?
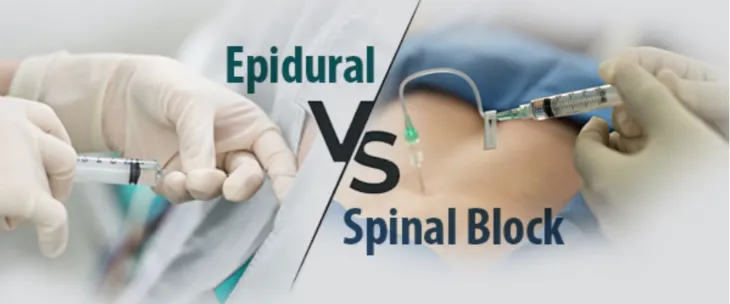
Anesthesia Awareness for Perioperative Nurses
Positive Psychology in psychiatric and mental health nursing practice
Resuscitation for Cardiac Arrest Should Begin and End with Basic Life Support
Teach Your Children CPR